For health systems, provider networks, and insurers, medical data integration is a strategic decision tied to delivery speed, compliance, and measurable outcomes. Your estate encompasses Electronic Health Records (EHRs), claims, labs, customer relationship management (CRM), and external sources. The real question is which pattern advances your goals at an acceptable cost and risk.
Your priority should dictate the pattern. Need fast testing of new digital solutions? Use application programming interface (API) layers, such as FHIR facades.
Aiming for durable quality and AI enablement? Consolidate into a clinical data repository (CDR) or a healthcare data integration platform.
Running multiple priorities at once? Adopt a hybrid approach: real-time clinical data orchestration at the edge, combined with extract, load, transform (ELT), and streaming into governed data stores.
If your goal is baseline interoperability, a healthcare IT integration engine may be sufficient without complete consolidation.
Learn more about what FHIR is in our recent article.
Edenlab helps leadership translate business goals into sustainable integration roadmaps. We align choices with the U.S. Office of the National Coordinator for Health IT (ONC), the Centers for Medicare & Medicaid Services (CMS), Germany’s Interoperable Systems in Hospitals (ISiK) specifications, and the European Health Data Space (EHDS). We also provide a technology foundation that enables our own product, the Kodjin Data Platform, to serve as a CDR or act as the integration backbone.
In this article, we will map common challenges of integrated healthcare systems to strategic integration approaches, explain where API layers, consolidation, or hybrids fit best, clarify trade-offs in time to value, quality, and risk, and show how to align health data integration with compliance and AI goals. So, you can move from quick data integration benefits to a durable platform.
Highlights:
- Integration decisions should align with business goals and measurable outcomes, rather than focusing on tools.
- APIs help you launch new digital services quickly and securely.
- A CDR builds trusted data for analytics and artificial intelligence.
- Use a hybrid model when you need to deliver both speed and long-term quality.
Need expert assistance with integration?
We are here to help. Check our
Healthcare integration solution development pageTechnical Approaches to Data Integration in Healthcare
Once the constraints are explicit, choose the model that aligns with today’s priority and tomorrow’s roadmap. There is no single winner. Fast digital delivery favors APIs and facades, while durable healthcare data quality favors consolidation; complex ecosystems often require a hybrid approach with orchestration. Edenlab’s role is to help you select, sequence, and deliver the mix that fits outcomes, regulations, and future readiness.
We have dual strengths and a clear playbook. For speed, we design application programming interface (API) layers and facades that let products ship without core disruption. For durable quality, analytics, and artificial intelligence, we consolidate data into governed platforms and CDRs. When needs are mixed, we plan hybrids that balance latency and reliability.
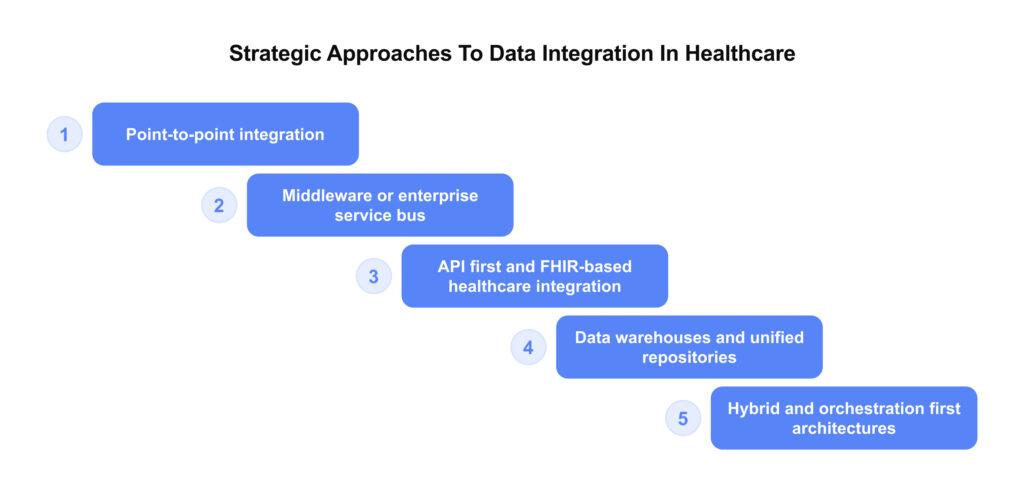
Point-to-point integration. Direct connections transfer data quickly between two systems and can resolve a pilot or urgent issue. They do not scale. Every change ripples, maintenance compounds, and topology drifts toward a spaghetti-like mess. Use sparingly with a retirement date and a plan to fold into shared services.
API-first (like FHIR-based) healthcare integration is one of the examples of this scenario. API layers expose stable, versioned contracts over clinical and administrative domains. FHIR facades enable teams to deliver new digital services without replacing core systems, promoting vendor-neutral interoperability. This is the fastest way to support partner ecosystems and external consumption. The trade-off is governance. Scopes, versions, and semantics must be actively managed to avoid creating another fragmented surface.
Middleware or enterprise integration bus. A central healthcare data ecosystem hub for integration orchestration normalizes formats, routes messages, and applies shared policies for validation, enrichment, and security. This suits estates with many legacy apps and event-heavy workflows. It reduces duplication and centralizes expertise but introduces runtime complexity and a single operational bottleneck. Ownership, observability, and regression testing are critical.
Data warehouses and unified repositories. A governed repository, also known as a CDR, consolidates standardized data for analytics, research, and population health. It improves quality and model performance and simplifies regulatory reporting. The time to first value is longer than with APIs, so consider consolidating pairs with targeted products and implementing phased onboarding. Protect health information using zone design, de-identification, or pseudonymization, and implement role-based access controls.
Hybrid and orchestration first architectures. Many programs need real-time coordination and durable consolidation. Combine an integration engine and orchestration middleware with batch ingestion for history/backfills and streaming ingestion for real-time events into a platform or CDR. Coordinate multi-step workflows, including eligibility, coverage rules, and clinical checks, without unnecessary duplication. You gain balanced latency and quality at the cost of operating two data speeds with tighter governance. This is often the safest path for complex provider and payer ecosystems.
A recent example of Edenlab’s contribution is an integration platform for patient-generated health data (PGHD) interoperability within the EHDS for the Ludwig Boltzmann Gesellschaft. The solution streams wearable data through Fitrockr, transforms it into FHIR resources with Kodjin mapping tools, and stores it in a cloud-hosted Kodjin FHIR Server on AWS. It supports real-time ingestion, GDPR-compliant consent management, and interoperability with EHRs, enabling scalable, standards-based use of wearable data for clinical and research teams.
Business Use Cases and Relevant Integration Patterns
Edenlab does the mapping work up front. We translate your priorities into domain contracts, phased onboarding, and a retirement plan for costly legacy links. As a result, you get faster product delivery, dependable reporting, and AI-ready datasets.
Below, we outline common scenarios and map each to the corresponding fitting integration pattern, along with its associated trade-offs.
Providers (hospitals and clinic networks)
| Business objective | Integration pattern |
| Fast digital launches (scheduling, telehealth, remote monitoring) | The integration pattern focuses on agility and interoperability rather than technology stack. The idea is to create a lightweight, vendor-neutral layer that connects new digital services with existing systems (EHRs, billing, communication) through unified data and security standards. This approach allows organizations to introduce new digital touchpoints and care workflows in weeks instead of months. |
| Care coordination and referrals across departments and partners | Use an integration engine with orchestration middleware to ensure orders, notes, and status updates are transmitted in real-time. This approach reduces duplicate work and missed appointments, but requires investment in tracing, replay, and contract tests to maintain high reliability. |
| Quality reporting and regulatory submissions | Deliver reports that regulators can trust every time. Use a governed Clinical Data Repository or unified platform with consistent codes and clear data origins. Onboard domains in phases, lock key definitions, and track changes. Build audit trails and reuse the same validated rules to prevent teams from rework. |
| Analytics and artificial intelligence readiness | Provide business teams with fresh, secure, and comprehensive data across all sources. Maintain clear zones for raw, standardized, and de-identified data, with strict access and consent controls in place to ensure confidentiality. Keep updates timely and publish well-described, model-ready datasets. Connect easily to external analytics and AI tools without having to reshape data every time. |
| Retiring brittle point-to-point interfaces | One-off links drain budgets through constant manual fixes, vendor lock-in, and “temporary” scripts that never die. Stabilize the edge with a custom orchestration middleware, allowing products to continue moving forward. The payoff is fewer incidents, lower support and license costs, and upgrades that don’t break everything. |
| Data as a product and secondary use | Package governed datasets for internal analytics, research, and partner consumption. Use a Clinical Data Repository (CDR) or governed platform with raw, standardized, and de-identified zones; expose versioned APIs or secure shares; publish catalogs and deprecation windows; assign product ownership and lifecycle. |
Payers (health plans and administrators)
| Business objective | Integration pattern |
| Member-360 and service personalization | Combine an API gateway, identity resolution, and event streaming so benefits and context are consistent at first contact; prevent fragmentation by maintaining a semantic catalog. |
| Claims adjudication and prior authorization automation | Orchestrate plan rules, coverage checks, and clinical context in one flow using integration middleware; you’ll cut manual review and avoidable appeals, but build in explainability for auditors and consumer-driven contract tests for each feed. |
| Quality reporting and regulatory submissions | Deliver reports that regulators can trust every time. Use a governed Clinical Data Repository or unified platform with consistent codes and clear data origins. Onboard domains in phases, lock key definitions, and track changes. Build audit trails and reuse the same validated rules to prevent teams from rework. |
| Value-based care | Run a hybrid approach: near-real-time ingestion for operational signals and consolidation in a platform/CDR for risk adjustment and quality. This approach provides balanced latency and reliability, albeit at the cost of operating two data streams with clear ownership and KPIs. |
| Accurate provider directory and routing | Drive contracting, credentialing, and availability updates through an evented API layer; directories stay current, and members route correctly, provided upstream systems are part of the product contract, not informal sources. |
| Regulatory assurance | The optimal integration pattern is a policy-driven data governance layer rather than a deep system overhaul. Existing claims, enrollment, and provider systems remain intact, while all inbound and outbound data flows pass through a unified compliance gateway that applies CMS-aligned validation rules. |
Build a future-ready integration backbone.
Review our
healthcare data integration services and schedule a consultation to learn moreThe hybrid integration model is a multi-functional solution
The hybrid integration model can address most of your business objectives simultaneously, cutting connector sprawl, reducing manual effort, and keeping sensitive data close to source while still powering analytics and AI.
This model combines these elements into one cohesive system.
- Orchestration middleware (integration engine). Coordinate real-time workflows across EHR, claims, pharmacy, imaging, and partner systems. Acknowledge the reality in hospitals today, on-prem routing, queues, and transformations.
- A cloud control plane with edge agents. Lightweight agents run near source and consumer systems to collect, buffer, validate, and send data up, while the cloud orchestrates and transforms, then returns results back through the same agents. This reduces custom connectors and centralizes change.
- API gateways with policy enforcement. Expose stable, versioned contracts for internal products and external partners, with scopes, consent, and access handled consistently.
- A consolidated platform for analytics and AI. Use a CDR or governed lakehouse to standardize semantics and power analytics and artificial intelligence, fed by streaming or ELT. Add data quality services and Master Data Management (MDM) to keep identities and codes consistent and to maintain documented data origins.
- AI assistants for integration operations. LLM–based helpers suggest mappings, detect schema drift, draft transformations, generate tests, triage quality issues, and automate safe retries with human-in-the-loop approval.
- Central governance with decentralized delivery. Keep identity, terminology, consent, and documented data origins in a shared core while domain teams own their APIs and event streams, so change stays fast and controlled.
Classic orchestration layers in providers are powerful but expensive to maintain because each route and transformation is hand-built. The hybrid model moves heavy transformation and coordination to the cloud, uses agents to simplify connections, and adds automation so teams stop writing every mapping by hand.
Key Challenges in Healthcare Data Integration
In this section, we revise common healthcare data integration challenges organizations face and offer some practical solutions to them:
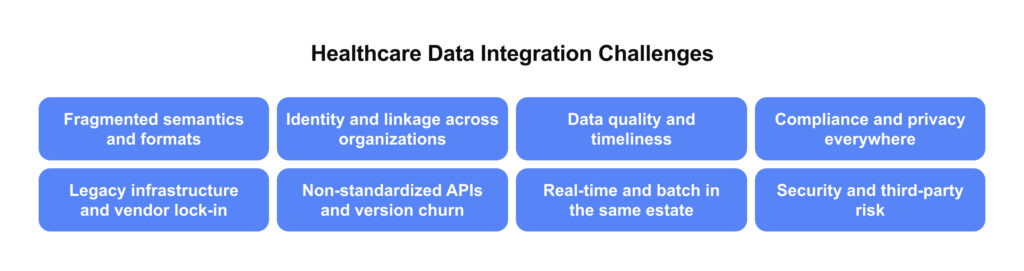
Fragmented semantics and formats
Most environments combine HL7 v2, CDA, various API styles, vendor-specific payloads, and custom files. Code systems differ across sources, and event messages often conflict with stateful records. Without a shared semantic layer and disciplined mapping, joins fail, measures skew, and analytics lose credibility.
What works: Establish a canonical model with governed FHIR profiles, a central vocabulary service, and a reusable mapping library. Normalize units, reconcile event-to-state with clear upsert rules, and treat mappings as versioned assets tested with contract and regression suites.
Identity and linkage across organizations
Patient, member, and provider identifiers rarely align across EHRs, payer platforms, labs, and apps. Probabilistic matching, a Master Patient Index (MPI), and directory reconciliation are challenging to implement at scale due to privacy constraints. Weak identity creates duplicates, misrouted referrals, and wrong attribution in value-based care.
What works: Deploy an enterprise MPI with deterministic and probabilistic rules, plus clerical review for edge cases. Set confidence thresholds and publish them. Maintain a governed provider directory. Use privacy-preserving record linkage, so the source data remains within its perimeter. Track match quality and feed fixes back to sources.
Data quality and timeliness
Late facts, missing fields, duplicate encounters, and mismatched timestamps are often encountered. Without schema evolution, teams cannot trust metrics or models. One-off reports accumulate, and nothing is reused.
What works: Define data contracts and Service Level Agreements (SLAs) for each domain. Add automated quality gates for completeness, conformance, and deduplication. Track the data’s path from the original source to the consumer. Use Change Data Capture (CDC) or event sourcing to cut drift. Version schemas and ship safe migrations.
Compliance and privacy everywhere
HIPAA and GDPR require least privilege access, consent enforcement, auditability, and defensible retention. These controls must hold across APIs, files, streams, temporary staging, and analytical stores. Cross-border data flows, vendor subprocessors, and evolving rules such as ONC or CMS updates, ISiK in Germany, and EHDS in the EU introduce new obligations that your architecture must absorb without stalling delivery.
What works: Implement policy-as-code for consent and access, combine role- and attribute-based controls, and segregate zones for raw, standardized, and de-identified data. Use pseudonymization and de-identification pipelines, centralize key management and secrets, and keep auditable trails for who accessed what, when, and why.
At Edenlab, we deliver compliance-heavy platforms at scale, including national infrastructure with thousands of users and multi-level access models.
We helped launch Ukraine’s National eHealth system, which was built from scratch and now serves over 36 million people. The HL7 FHIR–based, API-driven platform connects thousands of providers and pharmacies in real time. It supports clinical data exchange, electronic prescribing, referrals, and reimbursement workflows. To meet nationwide regulatory and security requirements, we implemented pseudonymization, machine learning (ML) driven deduplication, and fraud detection controls.
Legacy infrastructure and vendor lock-in
Core platforms may expose limited interfaces, rely on batch exports, or enforce proprietary models. One-off bridges multiply surface area and make change risky. Untangling this requires a stepwise path that stabilizes contracts at the edge while the core modernizes.
What works: Introduce FHIR or domain APIs as a facade, retire brittle point-to-point links, and backfill via ELT or CDC until core replacements are ready. Prioritize high-change, high-cost interfaces first, and insist on vendor-neutral formats.
Non-standardized APIs and version churn
Implementations vary across products, even when they follow a standard. Endpoints, fields, and behaviors drift, and versions move on different schedules. Without governance, semantic catalogs, and contract testing, an API first plan becomes a new integration tax.
What works: Govern profiles, publish a compatibility matrix, and enforce semantic versioning. Use consumer-driven contract tests and conformance testing in CI/CD, and provide deprecation windows with clear migration guides.
Real-time and batch in the same estate
Some workflows require sub-second orchestration, such as eligibility or prior authorization checks. Others thrive on nightly consolidation. Running both well requires clear SLAs, idempotency, back pressure handling, and replay strategies.
What works: Adopt a dual-speed architecture. Use streaming and an integration engine for low-latency paths, and a lakehouse or CDR for consolidation. Standardize correlation IDs, retries, dead-letter handling, and replay from an immutable log.
Security and third-party risk
Secrets management, key rotation, network segmentation, and zero trust patterns must be consistent across clouds, data centers, and vendor endpoints. Token scopes for APIs, least privilege roles for analytics, and continuous monitoring for exfiltration are table stakes.
What works: Apply attribute-based access control (ABAC) to data products, segment networks, and run continuous threat modeling and vendor assessments. Monitor for anomalous access and exfiltration with automated response playbooks.
Not sure where the bottlenecks are in your ecosystem?
Start with our deep dive on
health information exchange challengesWhy Choose Edenlab for Clinical Data Integration
Edenlab helps executives make the right strategy call, not just pick tools. We start with your business goals and map them to the right integration patterns: API layers and FHIR facades for speed, consolidation into a CDR or data platform for durable quality, and AI and hybrid, orchestration-first models when workflows span many systems or partners. Then we deliver end-to-end, architecture, build, governance, and run, so integration aligns with outcomes, regulatory demands, and future readiness.
Our own solution, Kodjin Data Platform, is a FHIR-centric platform proven as both a CDR and an integration backbone, combining versioned contracts, semantic mapping with terminology services, consent and de-identification, and documented data origins in a cloud-ready, vendor-neutral stack. Teams achieve fast, standards-based interoperability without being locked into a single vendor. We design for ONC and CMS requirements in the U.S., ISiK in Germany, and EHDS readiness in the EU, leveraging national-scale HIE experience and a proven track record with high-load, compliance-ready systems.
If you are weighing an API-first layer, a CDR-led consolidation, or a hybrid path, Edenlab will help you plan the sequence, quantify trade-offs, and deliver the platform that keeps you compliant today and ready for AI tomorrow.
Conclusion
Choosing an integration path is a strategy call. Match the pattern to the goal: APIs for speed, consolidation for data quality and AI, as well as orchestration when workflows span multiple systems. Remember, the hybrid approach can fit numerous use cases. Sequence them so that quick wins are achieved now, and the platform becomes stronger with each step.
Edenlab turns those choices into delivery. We help you set the roadmap, build the interfaces and platforms, and run them under clear governance. Our Kodjin Data Platform is a strong default for CDR and backbone use cases. Yet, we remain vendor-neutral when your stack calls for it. We also keep you aligned with regulatory expectations and audit needs at scale.
Make integration serve your strategy
We help provider and payer leaders map goals to the right patterns. We plan and deliver interface layers, clinical data repositories, and hybrid architectures with governance and compliance. Your roadmap balances delivery speed, data quality, and readiness for artificial intelligence.
FAQs
What’s the difference between HL7 and FHIR in integration?
HL7 Version 2 is a message-based standard, making it well-suited for hospital workflows. It facilitates the movement of events, such as admissions, orders, and results, between systems. FHIR is a modern, resource-based, and API-driven standard that supports REST, JSON/XML, as well as granular reads and writes. Most estates run both: keep HL7 v2 where it’s reliable and add FHIR APIs for partner apps, patient access, and fine-grained interoperability.
Is API-first integration always the best option?
API layers accelerate digital products and partner connectivity. They are not a cure-all. If your priority is data quality, analytics, or AI, a CDR or unified platform becomes more important. If workflows span multiple systems in real-time, an integration engine with orchestration is essential. For legacy estates, Middleware or an ESB often reduces duplication. API-only programs risk fragmentation unless paired with governance and a consolidation plan.
How do we ensure HIPAA compliance during integration?
Follow the principles of the Health Insurance Portability and Accountability Act (HIPAA), including the minimum necessary standard, informed consent, and accountability. Enforce role-based and attribute-based access control, encrypt data, keep audit trails, de-identify where possible, and sign Business Associate Agreements (BAAs).
What’s the timeline for a typical data integration project?
Work in phases: discovery, foundation, first domain, consolidation, and then scale-out. Deliver early value, expand by domain, and retire legacy links on a schedule.
Stay in touch
Subscribe to get insights from FHIR experts, new case studies, articles and announcements
Great!
Our team we’ll be glad to share our expertise with you via email









